

Patients simply do not advance to the operating room, for example, without a signed consent form. 6 Fortunately, in most cases, legal interpretation is pragmatic evidence of a good-faith effort to inform is usually found to be adequate.įor the sake of compliance, the informed consent document serves the administrative purpose of a systems-level check to ensure that a consent process has occurred. The Canadian Medical Protective Association provides detailed information on Canadian standards ( Even when the standard is clear, interpretation is required to apply the standard to a particular case thus, most litigation regarding informed consent focuses on precisely what information satisfies the applicable standard. Therefore, it is important for clinicians to determine the precise standard used in their jurisdiction and to adapt their practice accordingly.
Some jurisdictions use the reasonable person standard, whereas others continue to use the older standard of the reasonable physician.

However, the legal standards that apply to obtaining informed consent vary across jurisdictions, and their interpretation continues to evolve. The higher standard of informed consent further safeguards patients’ rights to autonomy, self-determination and inviolability. Legally, simple consent protects patients against assault and battery in the form of unwanted medical interventions. 4 Regardless of the standard used, informed consent is further predicated on the patient’s or surrogate’s capacity to make decisions - not only should the decision-maker understand the relevant information, he or she should also be able to appreciate the information’s importance and use it to weigh treatment options in light of their values. It was not until 1975 that American courts articulated the reasonable person standard, which required that physicians disclose the information that a “reasonable person” would want to know in a similar situation. Our bibliography includes randomized controlled trials, meta-analyses, systematic reviews, qualitative descriptions of patient and physician experience, and observational studies by sociologists and psychologists, in addition to books and articles that examine the law, ethics and policy of informed consent.Īlthough the concept of consent is rooted in ancient legal and philosophical precepts, the modern legal precedent for “simple” consent was written in 1914, establishing a patient’s “right to determine what shall be done with his body.” 2 The further obligation for physicians to disclose details about treatment in a process of informed consent did not emerge until the 1950s, 3 when courts first required physicians to disclose information customarily disclosed by experienced clinicians (e.g., the reasonable physician standard).

We noted that much of the literature on the topic of informed consent is descriptive and that there are a wide range of interventions and outcomes tested by the identified randomized comparisons.
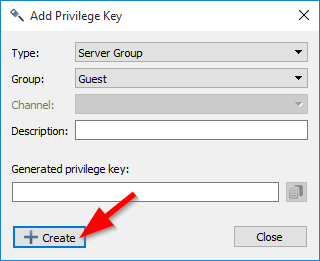
#Teamspeak channel privilege key cracker update
The recent systematic review by Schenker and coworkers, 1 in addition to our update of their search, found few “level 1” studies. However, the findings in these areas are transferable to other fields of medicine in which physicians must seek their patients’ consent for proposed treatment. The resulting bibliography reflects a bias within the literature toward surgery and other procedural disciplines such as gastroenterology, radiation oncology or interventional radiology. Focused Medline searches regarding specific aspects of informed consent were done as needed to address any gaps in our existing knowledge. The bibliography was expanded by adding related books and articles developed from reference lists, personal contacts, conference proceedings, and the coauthors’ bibliographies. This review is based on a broad Medline search for articles pertaining to informed consent in clinical settings, with a focus on surgery.


 0 kommentar(er)
0 kommentar(er)
